What is Neoplasia?
Neoplasia refers to the abnormal and unregulated growth of cells that results in the formation of a mass, commonly referred to as a tumor. Unlike normal cells, which grow and divide under precise regulation, neoplastic cells proliferate without the usual biological controls. This uncontrolled growth can create either benign (non-cancerous) or malignant (cancerous) tumors, with each type carrying different levels of risk. Neoplasia is a core concept in oncology (the study of cancer), and understanding it is fundamental to comprehending how cancers develop, progress, and respond to treatment.
In the human body, cell growth is a finely tuned process. Cells divide and multiply as needed, and old or damaged cells are removed through programmed cell death (apoptosis). In neoplasia, however, these natural processes break down. The term “neoplasia” itself stems from the Greek words “neo” (new) and “plasia” (formation), indicating the development of new, abnormal tissue that serves no functional purpose.
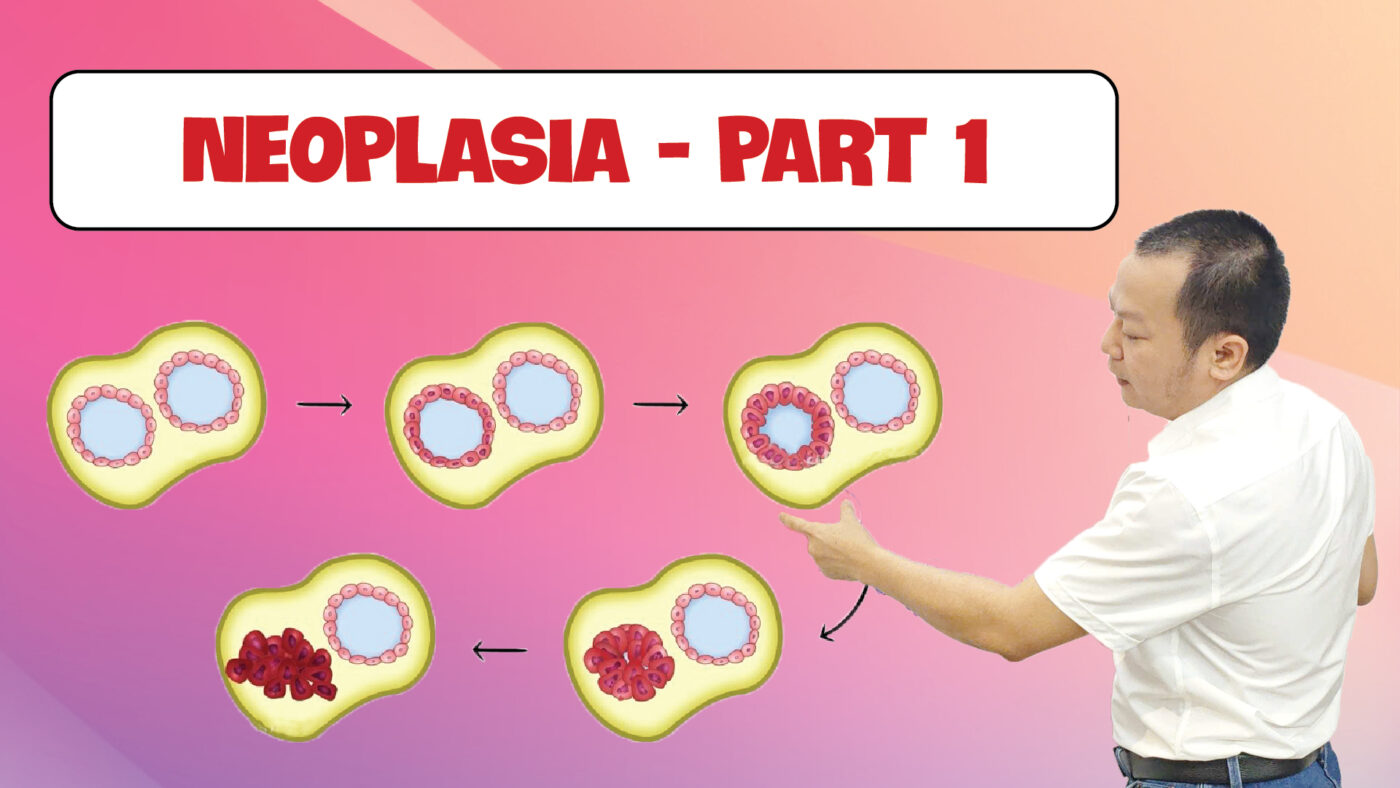
Key Stages of Neoplasia Development
The development of neoplasia is a multi-stage process that involves significant genetic and environmental influences. The stages through which neoplasia develops provide insights into how cancerous cells form and expand:
- Initiation: This first stage involves genetic mutations that affect a single cell. These changes may result from exposure to carcinogens (cancer-causing agents), such as tobacco smoke, radiation, certain chemicals, or even some viruses. Once a genetic mutation occurs, it can disrupt the cell’s normal growth and repair mechanisms.
- Promotion: In this stage, the mutated cell begins to divide uncontrollably. Unlike the initiation stage, promotion does not necessarily involve genetic changes but is marked by the rapid proliferation of cells. Promoters are agents that stimulate cell division, enabling the abnormal cell population to expand.
- Progression: During this phase, further mutations accumulate, and the growing cluster of cells starts to invade surrounding tissues. In malignant neoplasia, cells gain the ability to break away from the original mass and invade other parts of the body, a process known as metastasis.
- Metastasis: This is the spread of cancerous cells from the primary site to other areas, often through the bloodstream or lymphatic system. Once metastasis occurs, cancer becomes far more challenging to treat.
Causes of Neoplasia
Understanding the causes of neoplasia is critical in both prevention and treatment. While not all causes of neoplasia are preventable, many are influenced by lifestyle and environmental factors. Here are some of the most commonly identified causes:
- Genetic Predisposition: Inherited genetic mutations play a major role in some forms of neoplasia. For instance, mutations in the BRCA1 and BRCA2 genes are linked to breast and ovarian cancers. Individuals with a family history of cancer may have a higher risk of developing certain types of neoplasia due to inherited genetic factors.
- Environmental Factors: Carcinogens in the environment, such as radiation, pollution, and toxic chemicals, can lead to cellular mutations that trigger neoplasia. Industrial pollutants, radiation from the sun, and secondhand smoke are all examples of carcinogens.
- Lifestyle Choices: Smoking, alcohol consumption, and diet are significant contributors to cancer risk. Tobacco use is linked to lung, throat, and other cancers, while a diet high in processed foods and low in nutrients can increase susceptibility to various forms of cancer.
- Viruses and Infections: Certain viruses are known to be associated with cancer. For example, human papillomavirus (HPV) is linked to cervical and other genital cancers, and hepatitis B and C viruses are associated with liver cancer.
- Hormonal Imbalances: Hormonal influences are implicated in some cancers, such as breast, ovarian, and prostate cancer. The growth of hormone-sensitive cells can be influenced by hormonal fluctuations, which may contribute to neoplastic development.
Types of Neoplasia – Benign vs. Malignant Tumors
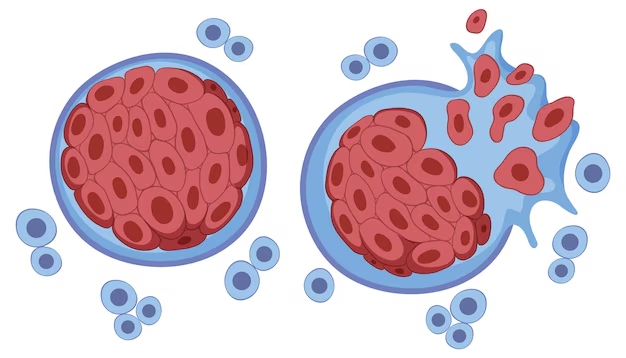
Tumors are generally classified into two main types: benign (non-cancerous) and malignant (cancerous). The primary distinction between them lies in their potential to invade neighboring tissues and spread to other areas of the body.
- Benign Tumors: These are usually harmless and do not invade surrounding tissues. Although they can grow to a substantial size and may cause pressure on adjacent organs, they do not metastasize. Examples of benign tumors include lipomas (fatty tissue growths), fibromas, and adenomas. Benign tumors can often be removed with surgery and usually do not recur.
- Malignant Tumors (Cancer): Malignant neoplasms are aggressive and invasive. They have the potential to invade nearby tissues and spread throughout the body (metastasis), posing a significant health risk. The ability to metastasize makes malignant neoplasia dangerous and challenging to treat. Common malignant neoplasms include carcinomas (originating in epithelial cells), sarcomas (in connective tissues), and leukemias (blood cancers).
Differences Between Benign and Malignant Neoplasia
Understanding the differences between benign and malignant neoplasia is essential for diagnosis and treatment planning:
- Growth Rate: Benign tumors typically grow slowly, while malignant tumors often grow more rapidly.
- Invasiveness: Benign tumors remain localized, whereas malignant tumors invade and destroy surrounding tissues.
- Metastasis: Malignant tumors can spread to distant organs through blood or lymph, a trait benign tumors lack.
- Cellular Appearance: Under a microscope, benign cells resemble normal cells, while malignant cells show irregular shapes, sizes, and disordered arrangements.
Mechanisms of Tumor Formation in Neoplasia
The formation of neoplastic cells involves a series of cellular and molecular changes that typically occur due to mutations in genes that control cell division and death. These mutations can be caused by both internal (genetic) and external (environmental) factors.
- Genetic Mutations: Mutations in tumor suppressor genes, such as p53 and RB, or oncogenes (genes that drive cell growth) like HER2 and MYC, can initiate neoplasia. Tumor suppressor genes act as “brakes” to cell growth, while oncogenes act as “accelerators.” When these genes mutate, the balance between cell growth and cell death is disrupted.
- External Influences: External factors like ultraviolet (UV) radiation, chemical exposure, and physical irritants can damage cellular DNA and activate oncogenes or deactivate tumor suppressor genes. These mutations may occur over a long period and gradually accumulate, eventually leading to neoplastic transformation.
Role of Genes in Neoplasia
Genes play a fundamental role in regulating cellular behavior. Here are key types of genes involved in neoplasia:
- Tumor Suppressor Genes: These genes act as the “brakes” of cell division. When they function normally, they help prevent uncontrolled cell growth. However, if these genes mutate, cells can grow unchecked. The p53 gene is one of the most well-known tumor suppressor genes.
- Oncogenes: Oncogenes are mutated versions of normal genes (proto-oncogenes) that promote cell division. When mutated, they can lead to excessive cell growth. Examples include the MYC gene, which is often overactive in various cancers.
- DNA Repair Genes: These genes help repair damaged DNA. Mutations in DNA repair genes, such as those found in some hereditary cancers, lead to an increased risk of neoplasia due to the accumulation of uncorrected DNA errors.
Diagnostic Methods for Neoplasia
Diagnosing neoplasia often involves a combination of imaging techniques, biopsies, and blood tests to detect abnormal cellular activity:
- Imaging Tests: X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) help visualize the size, shape, and location of tumors within the body. These tests are essential for initial diagnosis and staging.
- Biopsy: In a biopsy, a small sample of tissue is taken from the suspected tumor site and examined under a microscope. This procedure allows pathologists to determine whether the cells are benign or malignant.
- Blood Tests: Blood tests can detect cancer markers—substances in the blood that may indicate cancer presence. They can also reveal elevated white blood cell counts or other indicators of abnormal cellular activity.
Clinical Symptoms of Neoplasia
Symptoms of neoplasia vary depending on the tumor’s type, location, and size. Some common symptoms include:
- Localized Swelling or Lump: Tumors often present as lumps or swellings that are noticeable to the touch.
- Persistent Pain: Chronic or unexplained pain, especially if it worsens over time, can indicate neoplasia.
- Unexplained Weight Loss: Weight loss without changes in diet or exercise is often a red flag, especially in cases of advanced malignancies.
- Fatigue: Many cancer patients experience extreme fatigue, often due to anemia or other complications associated with cancer.
Treatment Options for Neoplasia
The treatment of neoplasia depends on multiple factors, including the tumor’s type, location, and stage. Standard treatment options include:
- Surgery: Often the first line of treatment, surgery involves physically removing the tumor. In cases where the tumor is benign, surgical removal may be curative. In malignant cases, surgery may be combined with other treatments to prevent recurrence.
- Radiation Therapy: Radiation uses high-energy rays to kill or damage cancer cells. It is commonly used to treat malignant tumors that cannot be fully removed surgically.
- Chemotherapy: Chemotherapy employs drugs to target and destroy rapidly dividing cells, a characteristic of cancerous cells. It can be systemic (affecting the entire body) or localized.
- Immunotherapy: Immunotherapy boosts the immune system’s ability to fight cancer. Drugs known as checkpoint inhibitors, for example, help immune cells recognize and attack cancer cells.
- Targeted Therapy: Targeted therapy uses drugs or other substances to precisely target specific molecules involved in tumor growth, minimizing damage to normal cells.
Importance of Early Detection in Treating Neoplasia
Early detection is critical for successful treatment outcomes. Regular screenings and monitoring for early signs of neoplasia can improve survival rates and reduce the severity of treatment required. Screening tests, such as mammograms, colonoscopies, and Pap smears, help detect cancer in its early stages when treatment is often most effective.
Conclusion
Neoplasia represents a complex and multi-faceted process that remains a central focus in medical research and clinical oncology. By understanding its causes, stages, and treatment options, medical professionals and patients alike can work toward early detection and effective intervention. Through advances in genetic research, diagnostics, and personalized treatments, the medical community continues to make strides in combating the challenges posed by neoplasia, offering hope for improved quality of life and outcomes for those affected.
Xem thêm video tại:
https://www.youtube.com/@learnabcacademy
Trang chủ LearnABC Education:
https://learnabcacademy.com/
Theo dõi thêm các bài viết tại:
https://huynhtrunutrition.com/
Hãy học cách phòng ngừa thay vì bệnh rồi mới tìm cách chữa trị. Tham khảo 2 tập của sách Ayurveda, link mua sách tại:
http://huynhtruayurveda.com
Câu hỏi thắc mắc, vui lòng liên hệ:
Facebook: https://www.facebook.com/LUYENPHATAM